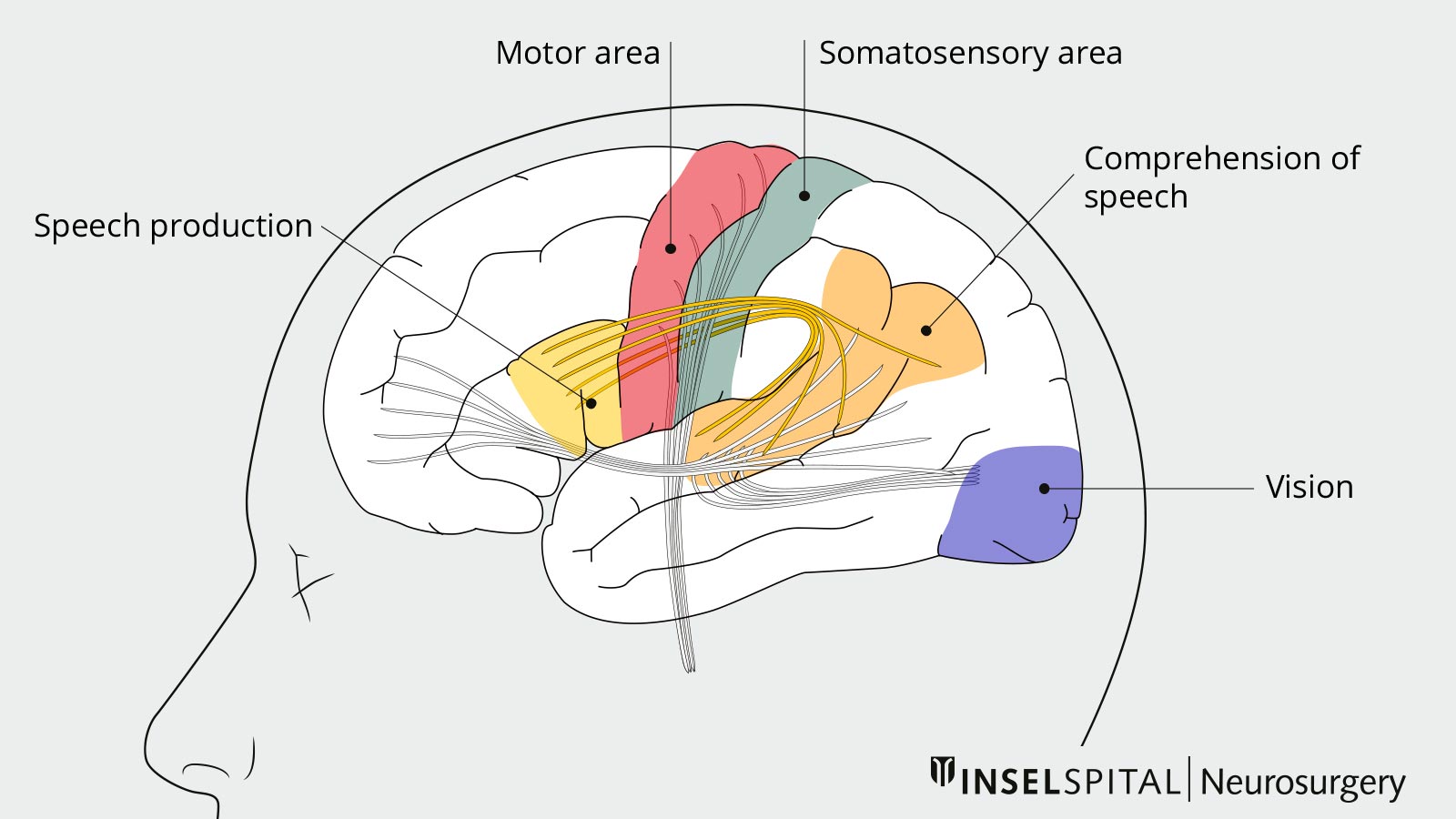
During brain tumor surgery, functions such as speech and vision cannot be reliably checked under general anesthesia. For operations near these functional centers, the patient is therefore awakened from anesthesia for brief tests. This method, known as awake brain surgery or awake craniotomy, allows tumors to be radically removed with maximum protection of brain functions, which is often not possible under general anesthesia.
Why should functional monitoring be carried out during brain surgery?
With many tumors of the brain, the boundary between the tumor itself and the surrounding brain tissue is not clearly visible. If the surgeon cannot see exactly where important brain functions are located around the tumor, he or she must maintain a safe distance, which inevitably leads to less complete removal of the tumor. Checking the functions in the gray area between the tumor and the healthy brain, on the other hand, helps to operate more safely and radically, as the surgeon now knows exactly where he can operate.
Are awake brain surgeries performed for all brain tumors?
Most tumors are located either near the brain's motor center or in areas of the brain whose functions can be compensated by other areas of the brain. In both cases, surgery and functional tests are performed under general anesthesia.
Brain functions such as speech or vision can only be tested when the patient is awake. For this reason, patients with a tumor near the speech or vision center of the brain are awakened from anesthesia during surgery for brief speech and vision tests. By identifying and precisely localizing these functions, the surgeon learns how far he can operate without endangering the patient's vision or speech. This means that brain tumors can also be removed more radically and safely in these areas *.
In the case of speech, an additional complication is that the brain shifts speech functions from the infiltration zone of the tumor to other areas of the brain in slow-growing brain tumors in order to preserve the ability to speak. This is known as plasticity. In concrete terms, this means that previously function-bearing areas of the brain lose their function due to the tumor infestation, while at the same time other healthy areas of the brain learn to take over. This plasticity makes it even more difficult to know where the language-relevant areas of the brain are located. This makes testing during surgery all the more important.
Before surgery
Awake brain surgery is a painless and safe operation. The patient is a member of the treatment team by showing the surgeon where and how the surgeon can operate through speech tests. In this way, the patient makes a significant contribution to the success of the operation. To ensure that this works, the patient is optimally prepared for awake brain surgery.
Some time before the operation, an outpatient neuropsychological assessment and training for the tests during the operation take place. The same person who carries out the speech or vision tests with the patient during the operation practises these relatively simple tests with them until they have mastered them.
Procedure of the surgery
For the operation, the patient's head is fixed in a holder. Although the brain is responsible for processing the perception of pain and for the sensation of pain, it has no sensory cells of its own to perceive pain and is therefore completely insensitive to pain. For this reason, local anesthesia of the skin is sufficient for awake craniotomy.
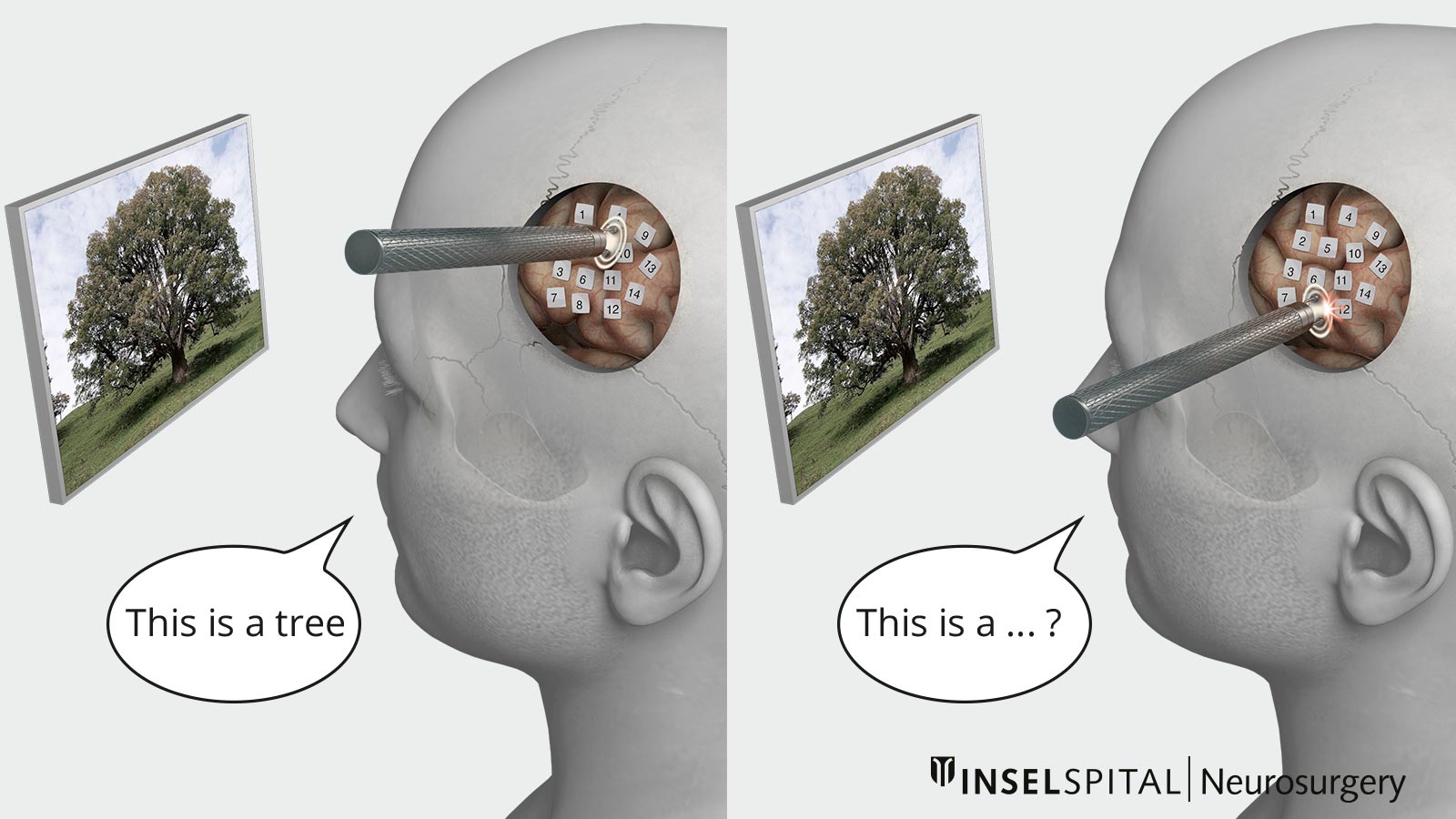
The first part of the procedure is performed under general anesthesia. The patient is only woken up after the skull has been opened with a special instrument. With the help of a special probe, the brain tissue is then scanned millimeter by millimeter while the patient performs the pre-rehearsed tests with the speech therapist. If there is a brief temporary disturbance of the tested brain function at a certain point, the surgeon knows that he must not operate here. The tumor can be removed from those areas where the tests are completed without any problems.
What tests are carried out during the awake surgery?
The specific tests carried out depend on the location of the tumor and individual patient factors, such as occupation, hobbies or other abilities *. This also includes the patient's language skills (up to 4 languages can be tested during the operation) as well as special skills such as arithmetic, spatial thinking or music-making. With the help of repetitive standardized tests, all these skills can be tested during the awake phase of the operation.

In this way, the brain tissue can be mapped by means of stimulation with microcurrents and the resection limits for the tumor can be determined. This process of brain mapping is also known as cortical mapping. Mapping is used to determine the entry points into the brain.
Repeated tests are also carried out in this way during the removal of the tumor (subcortical mapping) in order to protect the language pathways *,*,*,*. The tests take between 30 minutes and 2 hours, depending on the location and size of the tumor. Once the tests have been completed, general anesthesia is induced and the patient does not wake up until after the operation.
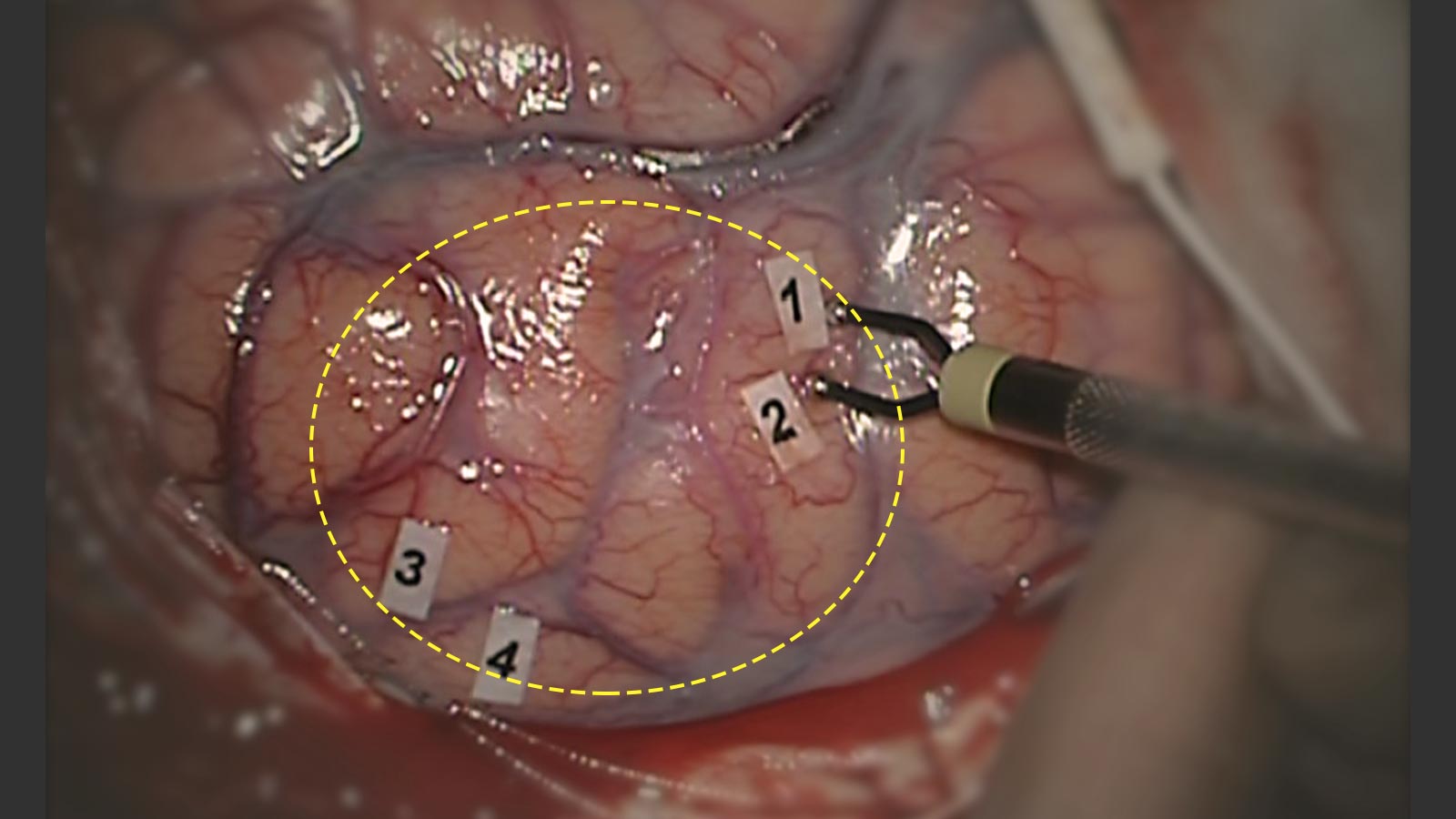
To prevent the electrical stimulation during the operation from causing an epileptic seizure, an intracranial EEG (electrocorticography) is recorded over the cortex. This allows seizures to be stopped before they become really noticeable.
After surgery
Postoperative phase
After the surgery, the patient is admitted to the monitoring ward for close observation and care. On the first or second day after the operation, a magnetic resonance imaging (MRI) scan of the brain is performed for postoperative control. Afterwards, the patient is transferred to the general ward.
Depending on the clinical condition, it will be decided in consultation with the patient and the specialists from physiotherapy, occupational therapy, and speech therapy whether the patient can return home or if inpatient rehabilitation is recommended.
Follow-up treatment
Regular MRI checks are part of the follow-up treatment. Due to the neuronal plasticity of the brain, brain functions may shift away from the area affected by the tumor over time. If the tumor increases in size again, a second awake brain surgery or alternatively radio- and chemotherapy can be considered *.
Who is eligible for awake brain surgery?
The patient's ability to cooperate is crucial to the success of awake brain surgery. This may be impaired or absent for medical or psychological reasons.
If speech is already impaired, the test may also provide incorrect results *.
For this reason, the indication for awake brain surgery is carefully determined and discussed with the surgeon, patient and speech therapist before the operation.
Why you should seek treatment at Inselspital
As numerous scientific publications have shown, intraoperative mapping of brain tissue can significantly reduce the occurrence of long-term neurological deficits after surgery. At the same time, mapping has significantly increased the number of complete and near-total tumor removals *,*,*,*.
At our Department of Neurosurgery, we have many years of experience in awake brain surgery with an interdisciplinary team of neurosurgeons, neurophysiologists, speech therapists, neuropsychologists and neuroanesthetists *.
Our clinic also took part in the first Europe-wide multicenter study in 2017 to assess intraoperative mapping and monitoring protocols in connection with the occurrence of peri- and intraoperative epileptic seizures. In this study, 41% of a total of 2098 patients underwent awake brain surgery. The study showed that clinics like ours, i.e. with a particularly high level of experience in intraoperative mapping, have a significantly lower risk of epileptic seizures during surgery *.
-
De Witt Hamer PC, Robles SG, Zwinderman AH, Duffau H, Berger MS. Impact of intraoperative stimulation brain mapping on glioma surgery outcome: a meta-analysis. J Clin Oncol. 2012;30:2559-2565.
-
Duffau H, Lopes M, Arthuis F, et al. Contribution of intraoperative electrical stimulations in surgery of low grade gliomas: a comparative study between two series without (1985-96) and with (1996-2003) functional mapping in the same institution. J Neurol Neurosurg Psychiatry. 2005;76(6):845-51.
-
Beez T, Boge K, Wager M et al. Tolerance of awake surgery for glioma: a prospective European Low Grade Glioma Network multicenter study. Acta Neurochir (Wien). 2013;155:1301-1308.
-
Chang EF, Clark A, Smith JS et al. Functional mapping-guided resection of low-grade gliomas in eloquent areas of the brain: improvement of long-term survival. Clinical article. J Neurosurg. 2011;114:566-573.
-
Schucht P, Beck J, Seidel K, Raabe A. Extending resection and preserving function: modern concepts of glioma surgery. Swiss Med Wkly. 2015;145:w14082.
-
Spena G, Schucht P, Seidel K et al. Brain tumors in eloquent areas: A European multicenter survey of intraoperative mapping techniques, intraoperative seizures occurrence, and antiepileptic drug prophylaxis. Neurosurg Rev. 2017;40:287-298.
