Functional neurosurgery deals with disorders that have no structural cause but are based on malfunctions of the nervous system. These include movement disorders such as Parkinson's disease or tremor, brain disorders such as epilepsy or Tourette's syndrome, and pain disorders such as migraine or cluster headaches. These diseases impair the quality of life, mobility, and independence of millions of people worldwide. Advances in research are enabling new therapies and better diagnoses, allowing those affected to lead more active and pain-free lives. With your support, you can help alleviate suffering and promote medical innovation.
Where does research into functional neurosurgery stand today?
Research into movement disorders, brain dysfunction, and pain disorders is making steady progress thanks to modern technologies and interdisciplinary approaches.
In the case of movement disorders such as Parkinson's disease, the focus is on biomarkers for earlier diagnosis and improved therapies such as deep brain stimulation (DBS) or focused ultrasound.
In the case of brain dysfunction such as epilepsy or depression, genetic analyses, innovative imaging techniques, and personalized neuromodulation are opening up new treatment options.
In pain research, central mechanisms such as neuroinflammation and neural plasticity are coming to the fore, while novel technologies such as AI and wearable devices are being used for personalized therapies.
Despite these advances, many questions remain unanswered, making continued support for research urgently needed.
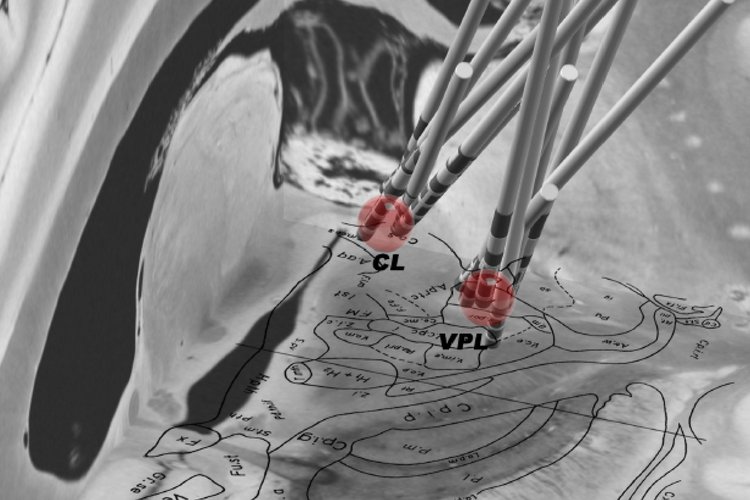
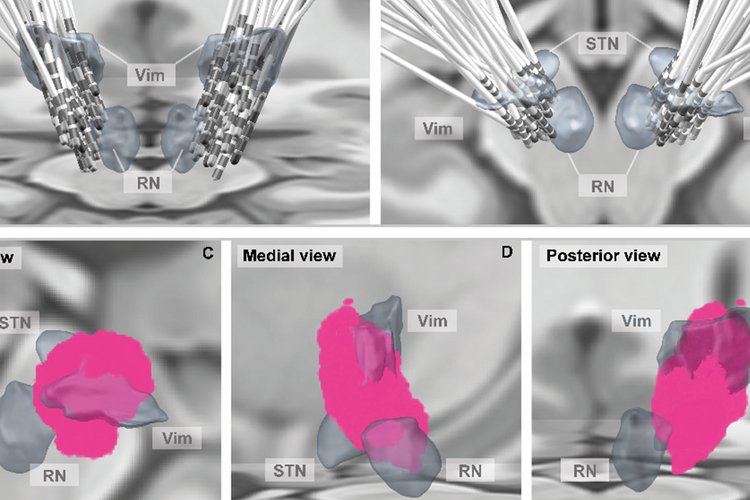
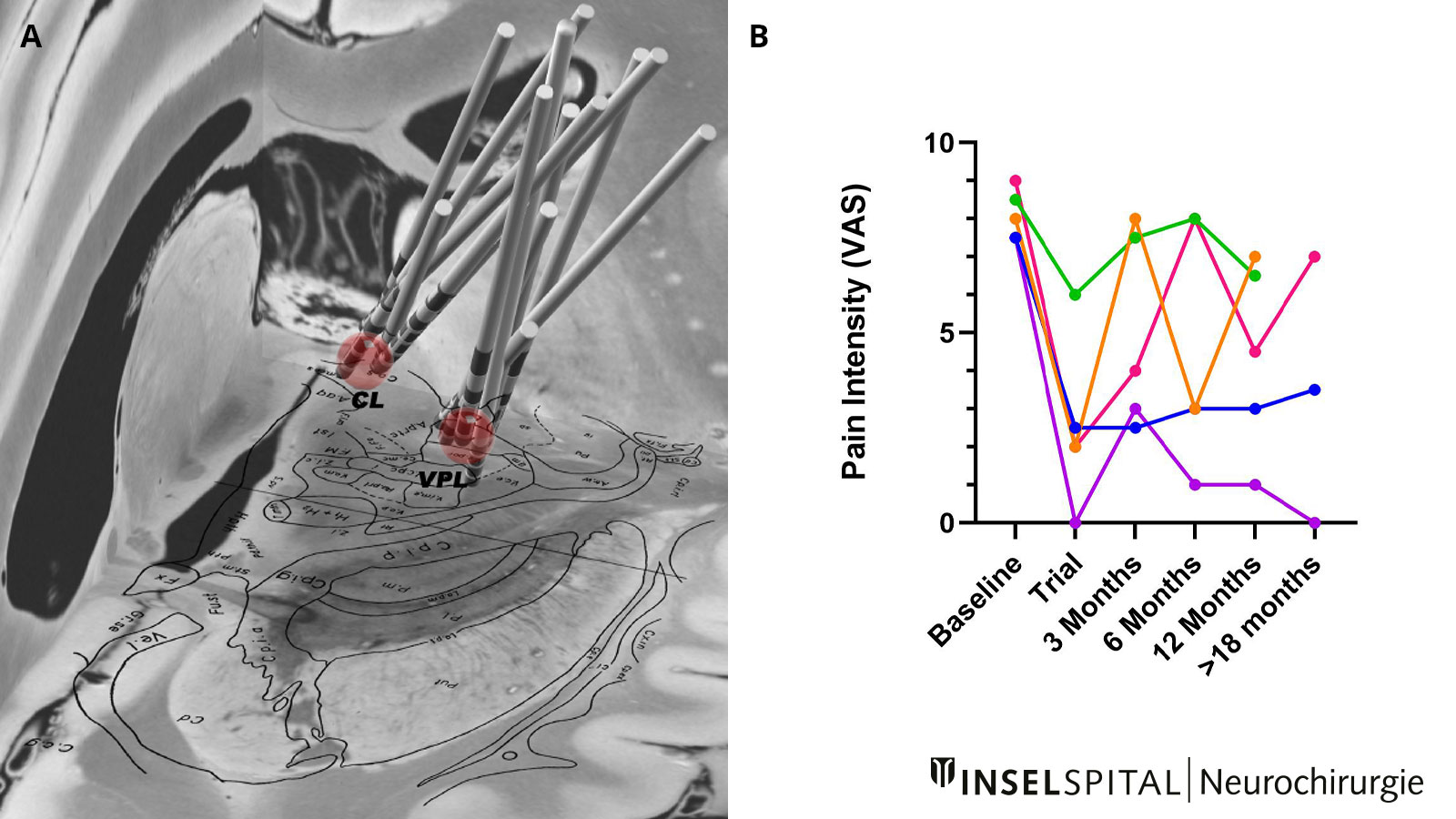
Burst DBS trial
Burst deep brain stimulation (DBS) for chronic neuropathic facial pain and neuropathic pain after stroke
Approximately 1–10% of all stroke patients develop chronic neuropathic pain syndrome, which often cannot be adequately treated with conventional therapies and medications. In these cases, there are alternative treatment methods such as deep brain stimulation. In this procedure, electrodes are implanted into specific anatomical structures of the brain to deliver therapeutic electrical impulses. Despite an initially good response to this therapy, many patients unfortunately experience a return of pain to the initial level over time.
In our research project, we now want to find out whether a new form of stimulation, known as burst stimulation, works well or just as well or better in patients with deep brain stimulation in the thalamus region.
| Head of study: | PD Dr. Andreas Nowacki, MD |
| Study coordinator: | Nicole Söll |
| Study identifyer: | NCT05204472 |
Post-stroke pain trial
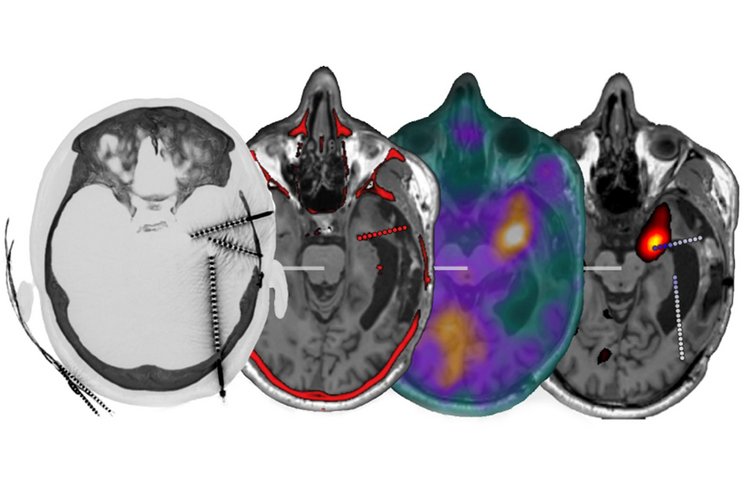
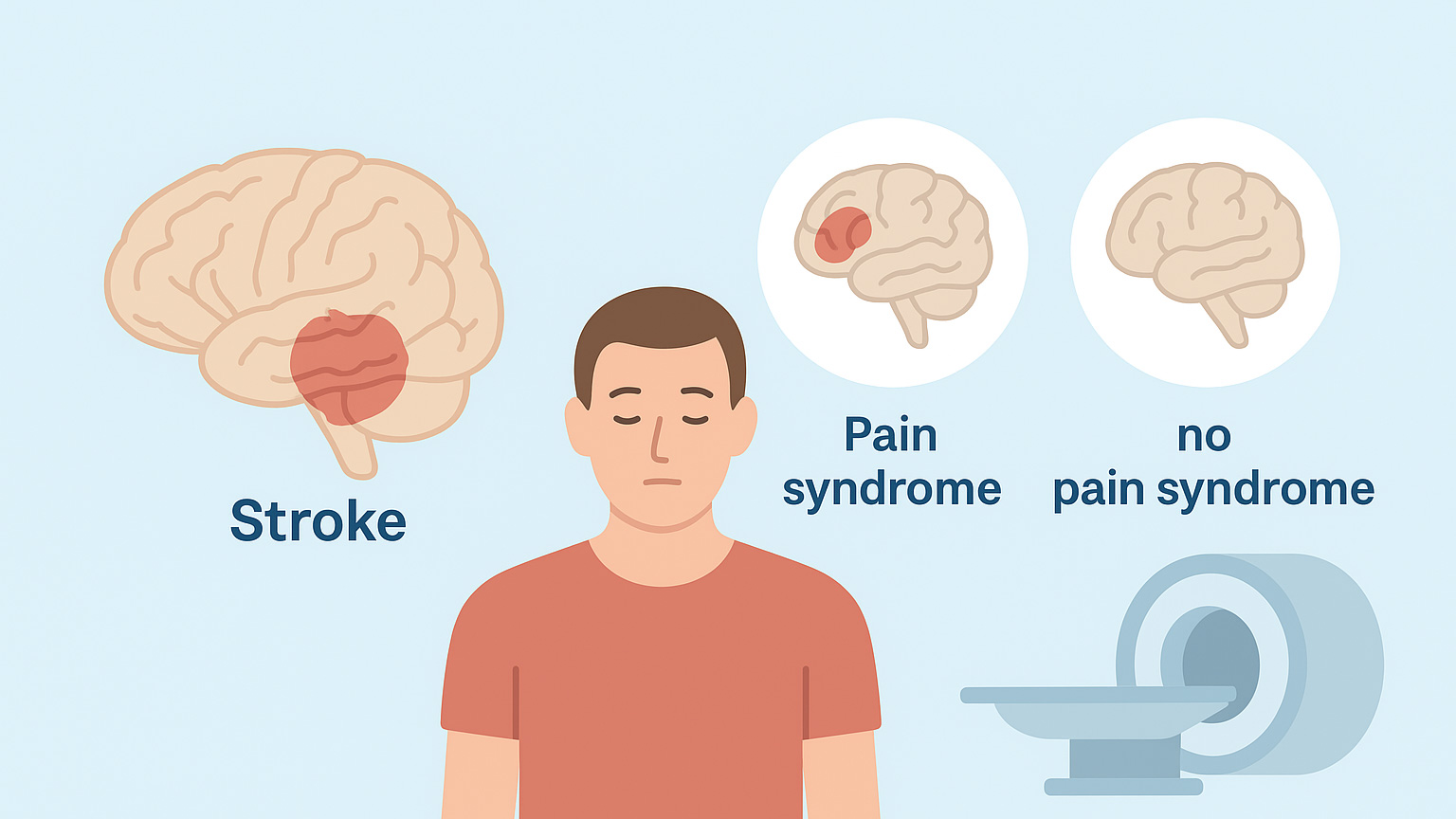
Neural reorganization in central pain syndrome after stroke: An fMRI study
After a stroke, some patients suffer from a specific pain syndrome that originates in the brain and is very difficult to treat. It is still largely unknown why only a small proportion of those affected develop such pain, even though the same regions of the brain are affected in many cases. In our study, we use modern magnetic resonance imaging to examine the brains of patients with similar stroke patterns – both those with pain and those without. In this way, we hope to gain a better understanding of the causes of this pain syndrome and find new approaches to provide more targeted help to those affected in the future.
| Head of study: | PD Dr. Andreas Nowacki, MD |
| Study coordinator: | Nicole Söll |
| Study identifier: | NCT05335668 |
| BASEC-No.: | 2020-02640 |
Project Flow driven endovascular electroencephalography (endoEEG) probes for epilepsy treatment
In this joint research project, Prof. Claudio Pollo (Neurosurgery, Inselspital), Prof. Maxime Baud (Neurology, Inselspital), and Prof. Mahmut Selman Sakar (Laboratoire de Systèmes MicroBioRobotiques, EPFL) are developing innovative endovascular EEG technologies for the precise localization of epileptic activity in the brain.
For the surgical treatment of drug-resistant epilepsy, the exact location of the epileptic seizures in the brain must be determined precisely and reliably in advance. A new method is being researched for this purpose: endovascular EEG (endoEEG). This involves measuring EEG signals via blood vessels in the brain, which is less invasive than previous methods using directly implanted electrodes.
The aim of the project is to show in preclinical experiments that this method:
- can reliably record brain signals from the motor cortex,
- detects epileptic seizures that have been specifically triggered, and
- can localize the epileptic focus very accurately.
In the long term, endoEEG should help to make epilepsy surgery safer and more precise.
The project is financially supported by the Swiss National Science Foundation (SNSF) and combines clinical expertise with cutting-edge engineering research.